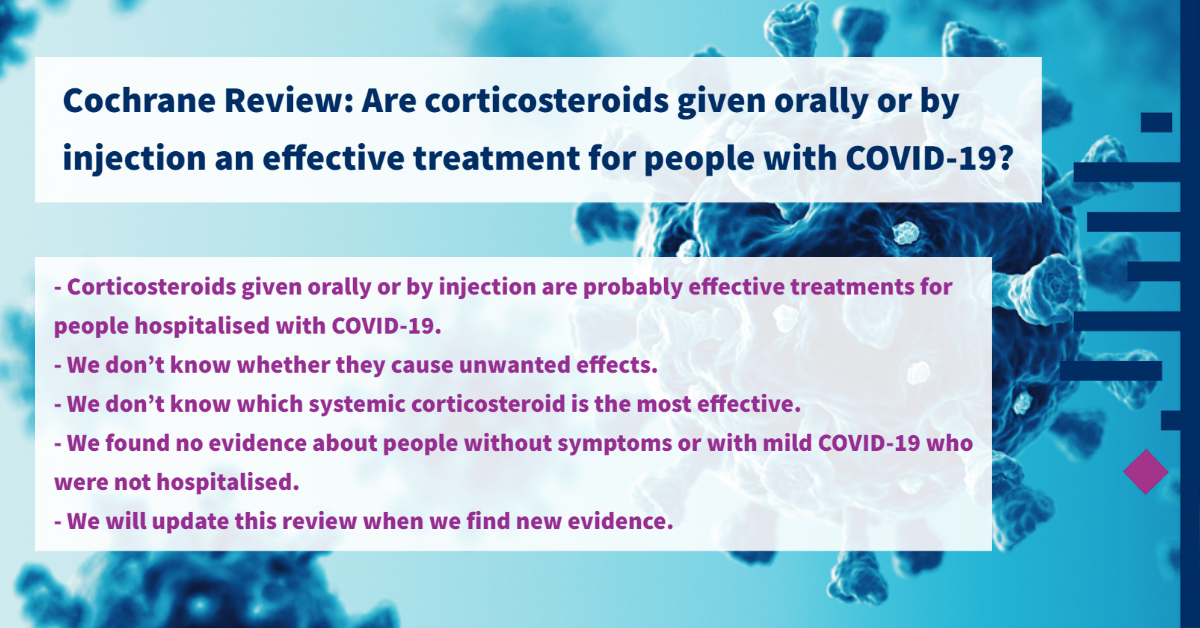
Key messages
- Corticosteroids (anti-inflammatory medicines) given orally or by injection (systemic) are probably effective treatments for people hospitalised with COVID-19. The authors don’t know whether they cause unwanted effects.
- The authors don’t know which systemic corticosteroid is the most effective. They found no evidence about people without symptoms or with mild COVID-19 who were not hospitalised.
- They found 42 ongoing studies and 16 completed studies that have not published their results. The authors will update this review when we find new evidence.
What are corticosteroids?
Corticosteroids are anti-inflammatory medicines that reduce redness and swelling. They also reduce the activity of the immune system, which defends the body against disease and infection. Corticosteroids are used to treat a variety of conditions, such as asthma, eczema, joint strains and rheumatoid arthritis.
Systemic corticosteroids can be swallowed or given by injection to treat the whole body. High doses of corticosteroids taken over a long time may cause unwanted effects, such as increased appetite, difficulty sleeping and mood changes.

Why are corticosteroids possible treatments for COVID-19?
COVID-19 affects the lungs and airways. As the immune system fights the virus, the lungs and airways become inflamed, causing breathing difficulties. Corticosteroids reduce inflammation, so may reduce the need for breathing support with a ventilator (a machine that breathes for a patient). Some patients’ immune systems overreact to the virus causing further inflammation and tissue damage; corticosteroids may help to control this response.
What did we want to find out?
The authors wanted to know whether systemic corticosteroids are an effective treatment for people with COVID-19 and whether they cause unwanted effects.
They were interested in:
- deaths from any cause up to 14 days after treatment, or longer if reported;
- whether people got better or worse after treatment, based on their need for breathing support;
- quality of life;
- unwanted effects and infections caught in hospital.
What did the authors do?
They searched for studies that investigated systemic corticosteroids for people with mild, moderate or severe COVID-19. People could be any age, sex or ethnicity.
Studies could compare:
- corticosteroids plus usual care versus usual care with or without placebo (sham medicine);
- one corticosteroid versus another;
- corticosteroids versus a different medicine;
- different doses of a corticosteroid; or
- early versus late treatment.
They compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did they find?
The team found 11 studies with 8075 people. About 3000 people received corticosteroids, mostly dexamethasone (2322 people). Most studies took place in high-income countries.
They also found 42 ongoing studies, and 16 completed studies that have not yet published their results.
Main results
Ten studies compared corticosteroids plus usual care versus usual care with or without placebo. Only one study compared two corticosteroids. The studies included only hospitalised people with confirmed or suspected COVID-19. No studies looked at non-hospitalised people, different doses or timing, or provided information about quality of life.
Corticosteroids plus usual care compared to usual care with or without placebo (10 studies)
- Corticosteroids probably reduce the number of deaths from any cause slightly, up to 60 days after treatment (9 studies, 7930 people).
- One study (299 people) reported that people on a ventilator at the start of the study were ventilation-free for more days with corticosteroids than with usual care, so corticosteroids may improve people’s symptoms.
- Four studies (427 people) reported whether people not on a ventilator at the start of treatment later needed to be put on a ventilator, but we could not pool the studies’ results, so we are unsure if people’s symptoms get worse with corticosteroids or usual care.
- The authors don’t know if corticosteroids increase or reduce serious unwanted effects (2 studies, 678 people), any unwanted effects (5 studies, 660 people), or infections caught in hospital (5 studies, 660 people).
Methylprednisolone versus dexamethasone (1 study, 86 people)
- The authors don’t know whether the corticosteroid methylprednisolone reduces the number of deaths from any cause compared to dexamethasone in the 28 days after treatment.
- The authors don’t know if methylprednisolone worsens people’s symptoms compared to dexamethasone, based on whether they needed ventilation in the 28 days after treatment.
- The study did not provide information about anything else we were interested in.
What are the limitations of the evidence?
The authors are moderately confident in the evidence about corticosteroids’ effect on deaths from any cause. However, their confidence in the other evidence is low to very low, because studies did not use the most robust methods, and the way results were recorded and reported differed across studies. The author team did not find any evidence on quality of life and there was no evidence from low-income countries or on people with mild COVID-19 or no symptoms, who were not hospitalised.
This evidence is up to date to 16 April 2021.
Lead authors explain the evidence
Lead Cochrane Haematology authors Carina Wagner from University of Cologne and Mirko Griesel from University of Leipzig Medical Centre said,
“Corticosteroids given orally or by injection probably have a small benefit in the treatment of people hospitalised with COVID-19, however we don’t know whether they also cause unwanted effects.
At this stage we don’t know which systemic corticosteroid is the most effective and we found no evidence about people without symptoms or with mild COVID-19 who were not hospitalised. We found 42 ongoing studies and 16 completed studies that have not yet published their results. We will update this review when we find new evidence about this treatment which is relatively low cost and available in large parts of the world.”
- Read the full review on the Cochrane Library
- Listen to the podcast in English and Spanish
- Read this news item in Malay
- Visit the Cochrane Haematology website
- See all the Cochrane COVID-19 resources

