In this interview with Dr. Lee Hooper we find out more about this new Cochrane review - Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease
Tell us about this Cochrane Review
There is a great deal of public belief in the cardiovascular benefits of omega-3 fats. Intakes of long-chain omega-3 fats in the US are higher from dietary supplements than foods. But public health advice differs across countries. The National Institute for Health and Clinical Excellence in the UK encourages people to eat oily fish intake (the major source of long-chain omega-3 fats) but discourages supplementation. The American Heart Association in the US also recommends eating oily fish and suggests that supplements may also be needed. We were interested in the evidence – are omega-3 fats protective, and how protective? We assessed effects of long-chain omega-3 fats give as oily fish and as supplements, and we also assessed effects of alpha-linolenic acid (ALA, the shorter chain omega-3 found in plant oils) given as foods or supplements.
It is an update, what has changed (studies, inclusion of new trial, quality of these trials)
We ran this update because three very large trials of several years’ duration assessing effects of long-chain omega-3 supplements on cardiovascular outcomes were published in late 2018 and early 2019. These boosted the numbers of people randomised into relevant trials for at least 12 months by over 30%, so had the potential to alter outcomes. This update includes 86 RCTs (162,796 participants) that randomised participants to either long-chain omega-3 or ALA for at least one year and assessed mortality or some form of cardiovascular disease. Including more participants, some of whom experienced cardiovascular events, has given us more power to see any effects of omega-3 fats on cardiovascular health.
Of the 86 included trials 28 were at low summary risk of bias (high quality trials), most trials gave supplements, and 19 trials gave supplements of at least 3g/d long-chain omega-3.
The 2018 review provided good evidence that taking long-chain omega 3 does not benefit heart health, risk of stroke or death. Is this still the case?
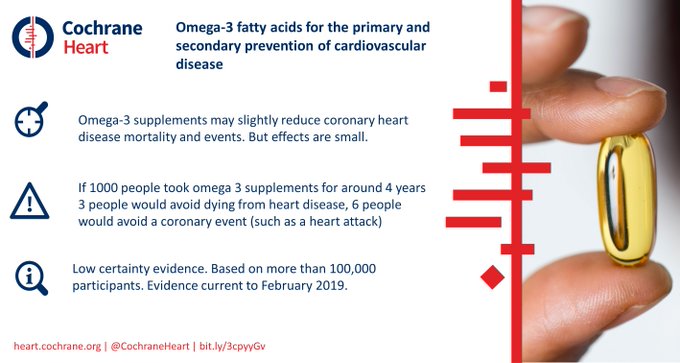
As in the previous version of this review, meta-analysis suggested little or no effect of increasing long-chain omega-3 on all-cause mortality, cardiovascular mortality, cardiovascular events, stroke or arrhythmia.
However, the update suggested that increasing long-chain omega-3 may slightly reduce coronary heart disease mortality and coronary heart disease events. These effects were very small. 334 people would need to take more long-chain omega-3 for several years for one person to avoid dying of coronary heart disease, and 167 people would need to take more to avoid one person experiencing a coronary heart disease event.
We wondered whether the effects of long-chain omega-3 fats would be greater in longer trials, or in studies giving higher doses. However, effects did not differ by trial duration or dose in pre-planned subgrouping or meta-regression.
Increasing long-chain omega-3 had little or no effect on serious adverse events, fatness, lipids or blood pressure, except increasing LCn3 reduced triglycerides by ~15% in a dose-dependent way.

How does this effect size, a Number Needed to Benefit (NNTB) of 167 or 334, compare with other medications used in cardiovascular disease prevention?
Simvastatin (a statin, or lipid-lowering medication) in secondary prevention: In the 4S trial, which enrolled people who had recently experienced myocardial infarction, 8% of the participants taking simvastatin died, and 12% of those taking the placebo died, a difference of 4%, so the NNTB was 25. Twenty-five people needed to take simvastatin for around five years to prevent one person dying. Most of us decide to take statins post-myocardial infarction.
Statins in primary prevention: The ten-year NNTBs for statins in primary prevention when used according to appropriate guidance are around 30. Thirty people need to take a statin for around 10 years so that one person does not experience atherosclerotic cardiovascular disease.
Ezetimibe (a cholesterol absorption inhibitor) in secondary prevention: If 50 people with acute coronary syndrome take ezetimibe in addition to statin for seven years one person will avoid a cardiovascular event.
These are the numbers that we associate with effective drugs – NNTBs of 25 to 50. Many more people need to take a long-chain omega-3 supplement to prevent a single coronary heart disease event or death. Long-chain omega-3 fats are much less effective than these drugs (with NNTBs of 167 or 334), and almost all the people who take the supplements will not gain from them.
Have the conclusions changed around oily fish? Is it protective of our hearts?
Sadly, we didn’t find any additional trials that increased the amount of oily fish that participants ate. That means that we still don’t fully understand the effects of eating more oily fish on cardiovascular health. Fish and seafood are nutrient-dense and rich in a variety of other nutrients (such as vitamin D, calcium, iodine, selenium, protein) so are useful foods even without cardiovascular benefits.
What are the effects of the vegetarian /vegan version of omega-3, ALA?
Increasing ALA intake probably makes little or no difference to all-cause mortality, cardiovascular mortality, coronary heart disease mortality and coronary heart disease events. However, increased ALA may slightly reduce risk of cardiovascular disease events and arrhythmia. Again, these effects are small: 500 people would need to increase their ALA intake for several years to prevent one person experiencing a CVD event, and 91 people would need to increase ALA to prevent one person experiencing arrhythmia.
Are there plans to update this review again soon?
The review will need to be updated once further large and high-quality trials of eating oily fish and/or increasing ALA intake are available. We hope that is soon. There are no further very large trials of long-chain omega-3 supplements underway that will trigger update automatically, though some large trials may make further outcome data available.