
Coronavirus (COVID-19) is a new respiratory infectious disease that has spread quickly throughout the world. Healthcare workers treating patients with COVID-19 are at risk of infection themselves through droplets from coughs, sneezes or other body fluids from infected patients and contaminated surfaces.
This review is one of a series of rapid reviews that Cochrane contributors have prepared to inform the 2020 COVID-19 pandemic. The aim of this Cochrane review of qualitative research (“qualitative evidence synthesis”) is to explore factors that influence whether healthcare workers follow infection prevention and control (IPC) guidelines for respiratory infectious diseases. To answer this question, the authors searched for and analysed qualitative studies about this topic.
Healthcare workers point to several factors that influence their ability and willingness to follow IPC guidelines when managing respiratory infectious diseases. These include factors linked to the guideline itself and how it is communicated, support from managers, workplace culture, training, physical space, access to and trust in personal protective equipment (PPE), and a desire to deliver good patient care. The review also highlights the importance of including all facility staff, including support staff, when implementing IPC guidelines.
When respiratory infectious diseases become widespread, such as during the COVID-19 pandemic, healthcare workers’ use of IPC strategies become even more important. These strategies include the use of PPE such as masks, face shields, gloves and gowns; separating patients with respiratory infections from others; and stricter cleaning routines. Exploring how healthcare workers view and experience these strategies can help authorities and healthcare facilities learn more about how best to support healthcare workers to implement them.
The authors found 36 relevant studies and sampled 20 of these studies for analysis. Ten studies were from Asia, four from Africa, four from North America and two from Australia. The studies explored the views and experiences of nurses, doctors and other healthcare workers when dealing with SARS, H1N1, MERS, tuberculosis, or seasonal influenza. Most of these healthcare workers worked in hospitals; others worked in primary and community care settings.
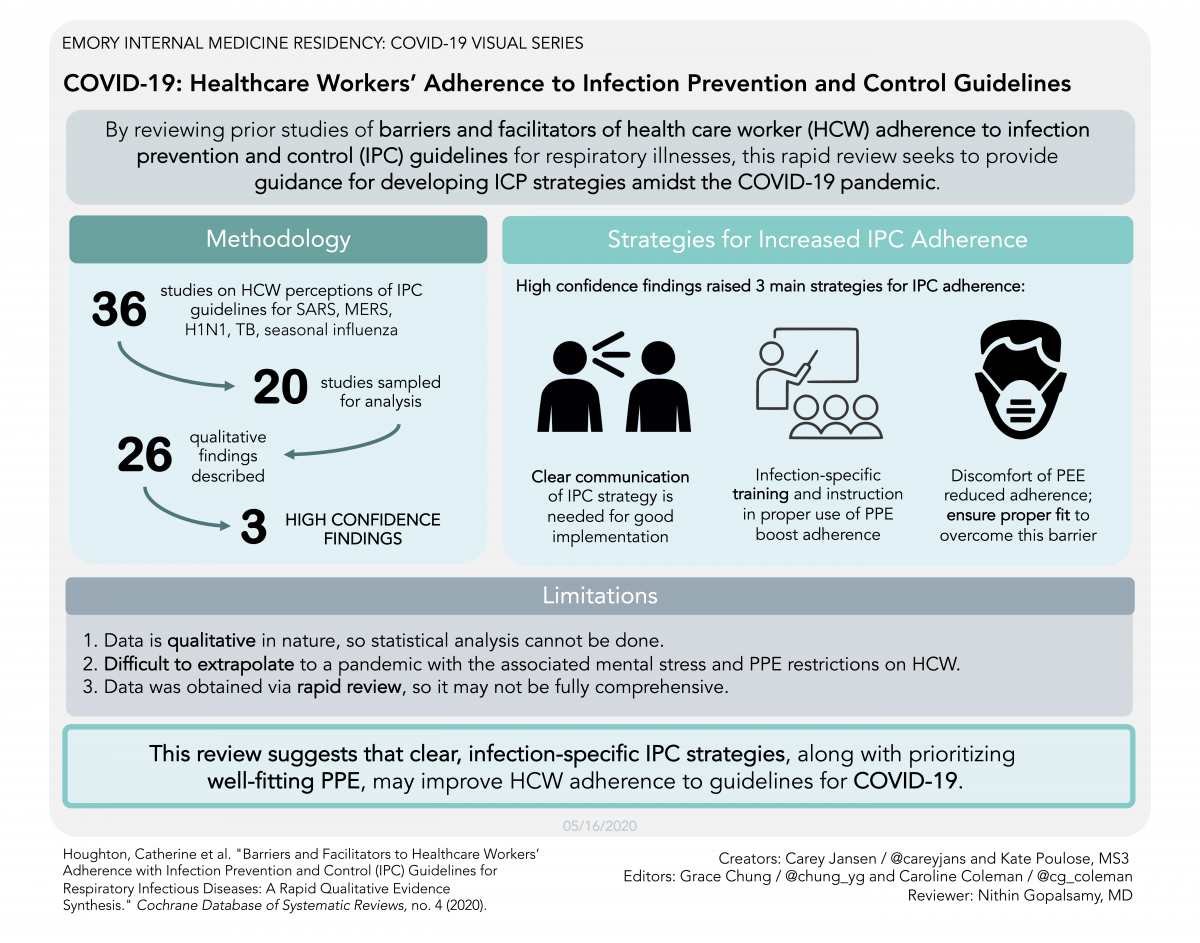
The review pointed to several factors that influenced healthcare workers’ adherence to IPC guidance. The following factors are based on findings assessed as of moderate to high confidence.
- Healthcare workers felt unsure when local guidelines were long, unclear or did not match national or international guidelines. They could feel overwhelmed because local guidelines were constantly changing. They also described how IPC strategies led to increased workloads and fatigue, for instance because they had to use PPE and take on additional cleaning. Healthcare workers described how their responses to IPC guidelines were affected by the level of support they felt they received from their management team.
- Clear communication about IPC guidelines was seen as vital. But healthcare workers pointed to a lack of training about the infection itself and about how to use PPE. They also thought it was a problem when training was not compulsory.
- Having enough space to isolate patients was seen as vital. Too few isolation rooms, anterooms (small rooms leading from a corridor into an isolation room) and shower facilities was a problem. Other important practical measures described by healthcare workers included minimising overcrowding, fast-tracking infected patients, restricting visitors, and providing easy access to handwashing facilities.
- A lack of PPE, or PPE that was of poor quality, was a serious concern for healthcare workers and managers. They also highlighted the need to adjust the amount of supplies as infection outbreaks continued.
- Healthcare workers believed that they followed IPC guidance more closely when they saw the value of it. Other healthcare workers felt motivated to follow the guidance because of fear of infecting themselves and their families, or because they felt responsible for their patients. Some healthcare workers found it difficult to use masks and other equipment when it made patients feel isolated, frightened or stigmatised. Healthcare workers also found masks and other equipment uncomfortable to use. The workplace culture could also influence whether healthcare workers followed IPC guidelines or not.
- Across many of the findings, healthcare workers pointed to the importance of including all staff, including cleaning staff, porters, kitchen staff and other support staff when implementing IPC guidelines.
- Read the full Cochrane Review
- Read this news item in Traditional Chinese or in Malay
- Listen to the podcast in English and Croatian
- Evidence Summary for ministries of health, healthcare facilities and other stakeholders to plan, implement and manage IPC strategies for respiratory infectious diseases (also available in French, Spanish, Portuguese, and Norwegian)
- One page infographic ministries of health, healthcare facilities and other stakeholders to plan, implement and manage IPC strategies for respiratory infectious diseases (Evidence Synthesis Ireland and Cochrane Ireland, April 2020, contact: esi@nuigalway.ie)
- Read the Evidently Cochrane blog post 'Personal protective equipment (PPE) for healthcare workers: new Cochrane evidence'
- Visit the Cochrane Effective Practice and Organisation of Care website
- Read all the Cochrane resources and news on COVID-19
