
Chantale Dumoulin and Licia Cacciari from Cochrane Incontinence wanted to find out if pelvic floor muscle training (PFMT) helps women with urinary incontinence problems. They did this by comparing the effects of this training with no treatment, or with any inactive treatment (for example, advice on management with pads). We asked Chantale and Licia questions about this recent Cochrane Review.
Please can you describe yourself and your Cochrane Group?
Since 2012 I have held a Canada Research Chair in Urogyneacological Health and Aging. Our research program's overarching goal is to improve continence care in older Canadian women. With this goal in mind, I partnered with a New Zealand expert in pelvic floor rehabilitation reviews; Dr. J. Hay-Smith and a post-doctoral fellow and physiotherapist from Brazil, Dr Licia Cacciari, to update our knowledge of the effectiveness of pelvic floor rehabilitation for urinary incontinence, in women. Conducting this review update will help inform my research program but most importantly will transfer the evidence to patients, clinicians and researchers with the overall goal to improve continence care in women.
What was the background to the Review?
Stress incontinence is leaking of urine which cannot be easily controlled (if at all) when performing a physical activity. Physical activities could include coughing, sneezing, sporting activities or suddenly changing position. Urgency incontinence happens with a sudden, strong need to urinate. This can often lead to not making it to the toilet in time to urinate, resulting in leakage. Mixed incontinence is where someone has both stress and urgency incontinence.
A wide range of treatments have been used in the management of urinary incontinence, including conservative interventions (such as physical therapy, lifestyle intervention, behavioural training and anti-incontinence devices), pharmaceutical intervention and surgery. This review focuses on one of the physical therapies, specifically pelvic floor muscle training (PFMT).
Pelvic floor muscle training is a program of exercises to improve pelvic floor muscle strength, endurance, power, relaxation or a combination of these. It is a widely used treatment for women with stress, urgency and mixed incontinence.
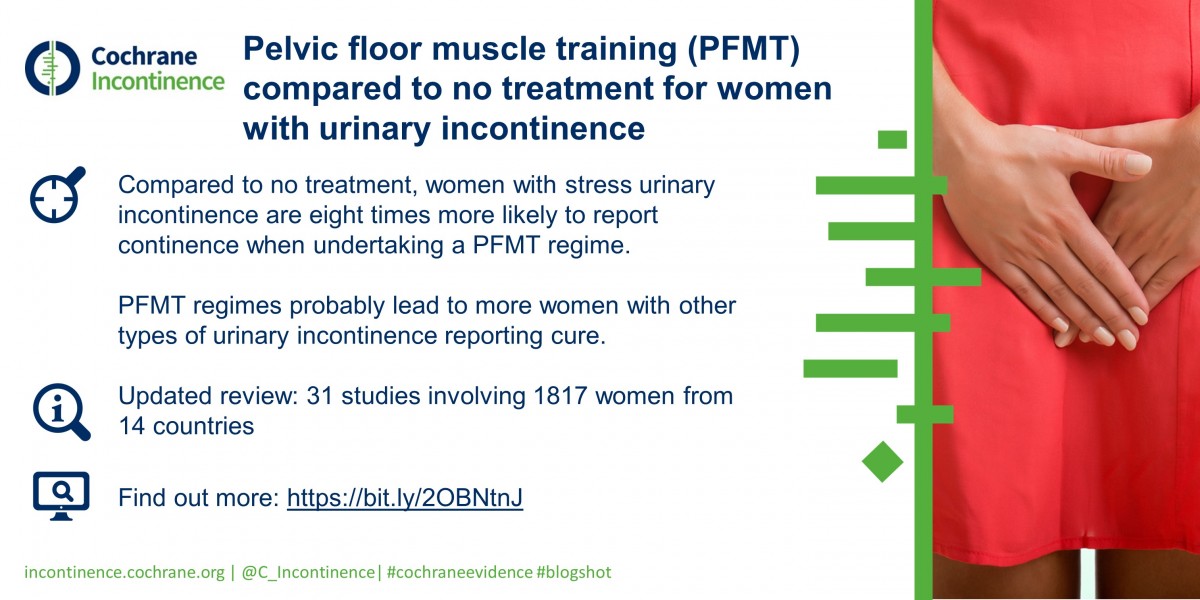
We wanted to find out if PFMT helps women with urinary incontinence problems. We did this by comparing the effects of this training with no treatment, or with any inactive treatment (for example, advice on management with pads). We also summarized findings on costs and cost-effectiveness.
What has changed in this update?
In this update we included ten new trials, which did not change the essential findings of the prior review. However, the wider range of populations, countries and secondary outcomes within these new trials emphasized the strength of recommendation of PFMT for women with urinary incontinence. There is now one report of reduction of urinary leakage episodes for women with urgency urinary incontinence treated with PFMT and one report of better quality of life for women with mixed urinary incontinence treated with PFMT.
Of note, in almost all new included trials, the PFMT protocols were described in more detail, with progressive training based on exercise physiology. Grade A patient-reported symptoms and quality of life outcomes were used more often, in line with recent international guidelines recommendations. Finally, we are starting to gather data supporting PFMT cost-effectiveness and the results look promising.
Why was it important to conduct this Review?
Earlier Cochrane Reviews of PFMT are outdated as new trials have been published. There is sufficient uncertainty about the effects of PFMT to suggest that continuing to update earlier Cochrane reviews is warranted.
What are the main implications of this research?
This Review is important for clinicians and consumers. Based on the data available, we can be confident that PFMT can cure or improve symptoms of stress incontinence and all other types of UI. It’s also important to note that negative side effects of performing PFMT were rare and, in the two trials that did report them, the side-effects were minor.
This Review is also important for researchers, since it highlights the need for more pragmatic, well-conducted and explicitly reported trials comparing PFMT with control to investigate the longer-term clinical effectiveness and cost-effectiveness of PFMT for women with symptoms of stress, urgency and mixed urinary incontinence.
What would you like to see happen as a result of publishing this Review?
The findings of the review suggest that PFMT could be included in first-line conservative management programs for women with urinary incontinence. Clinicians and health care providers should be aware of this evidence.
